Abstract
Background There is increasing evidence supporting the use of palliative care in the management of both solid and hematologic malignancies. As an integral part of oncologic care, palliative care has been reported to improve survival in diverse malignancies. Our study aimed to describe trends in the utilization of palliative care in diffuse large B cell lymphoma (DLBCL) patients.
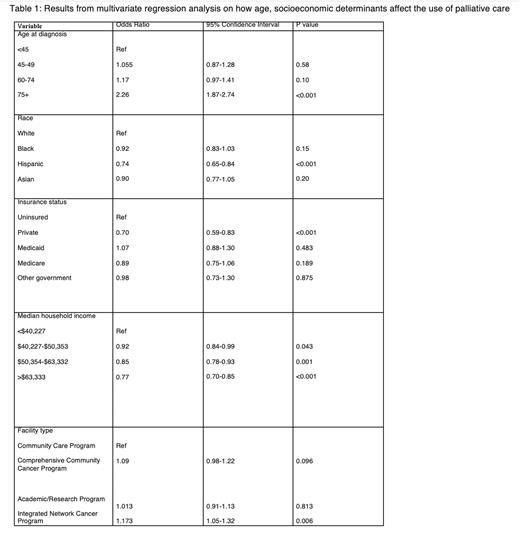
Methods Patient-level data of patients with DLBCL reported between 2004 to 2019 was extracted from the National Cancer Data Base (NCDB). After excluding 1173 patients with unknown palliative care status, we included 264,549 patients in our analyses. Chi-square tests were used to assess the characteristics of palliative care recipients and non-recipients. Multivariate logistic regression was used to identify the variables which influenced the likelihood of receiving palliative care. Age (<45, 45-59,60-74, 75+), sex (male and female), race (Hispanics, Whites, Blacks, Asian), Charlson-Deyo comorbidity score, insurance status (uninsured, private insurance, Medicare, Medicaid, other government), median household income (<$40227, $40227-$50353, $50,354-$63332, >$63333), educational status (as specified by the database), facility type (community, academic, comprehensive and integrated cancer centers), and year of diagnosis (2004-2007, 2008-2011, 2012-2015, 2016-2019) were variables included in our study. Statistical analyses were performed using SPSS.
Results Of 264,549 DLBCL patients, 3.2% (n=8460) utilized palliative care. The utilization of palliative care increased significantly from 2004-2007 to 2016-2019 (2.6% vs 3.71%, p < 0.001). A greater proportion of patients older than 75 years old received palliative care than those younger than 45 years old (5.09% vs 1.66% p<0.001). Patients of Hispanic origin were less likely to receive palliative care compared to Whites (OR 0.74, 95% CI 0.65-0.83). No statistically significant difference in palliative care utilization was found between Whites and other non-Hispanic groups. Privately insured patients had the lowest palliative care utilization amongst all insurance groups and these patients were less likely to receive palliative care compared to uninsured patients (OR 0.70, 95% CI 0.59-0.83). The odds of receiving palliative care were higher at integrated cancer centers than at community care programs (OR 1.17, 95% CI 1.05-1.32). DLBCL patients from households with a median income of >$63,333 were less likely to receive palliative care than those from low-income (<$40,227) households (OR 0.77, 95% CI 0.70-0.85).
Disclosures
Armitage:Cardiff Oncology: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal